SMART-EST Goals for Patient Nutrition and Lifestyle Changes
Lee Luetkemeyer, MHS, PA-C
PA Foundation Nutrition Outreach Fellow
Director of Didactic Education and Assistant Professor, University of Oklahoma-Tulsa School of Community Medicine PA Program
May 12, 2023

I serve as director of didactic education and assistant professor at the University of Oklahoma-Tulsa School of Community Medicine PA Program. In addition to my day-to-day role, I was selected to serve as a 2022-2023 Nutrition Outreach Fellow with the PA Foundation. As a Fellow, I have been able to expand my knowledge about nutrition and gain experience leading nutrition outreach to community members, PA students, and healthcare providers.
Any PA will tell you that nutrition plays a monumental role in the development and management of disease. While we recognize this connection, many providers may not feel comfortable discussing the role of nutrition with patients. This can be due to limited nutritional knowledge as well as the time constraints of a busy clinic schedule. Historically, instruction on nutrition has been lacking in medical education.1 Today, PA programs and medical schools are expanding didactic coverage of nutrition, giving new learners more information to share with future patients. Programs like the PA Foundation’s Nutrition Outreach Fellowship and the AAPA Nutrition Toolkit2 allow practicing PAs to gain additional knowledge on nutrition that equips them to facilitate effective conversations with patients and cultivate positive health outcomes.
As an educator, I want students to recognize and feel confident discussing the role of nutrition in patients’ lives. This year, through participation in the Nutrition Outreach Fellowship, I have been able to expand didactic training on nutrition as it relates to diabetes, wound healing, and healthy aging in particular. Students who participate in this training will be able to apply their new insights on these topics when they start clinical rotations this fall.
I also work in a family medicine clinic that provides care to underserved patients. All of my patients have chronic diseases, many of which are influenced by nutrition. Diabetes and obesity are two of the most common diagnoses I see in clinic. In fact, Oklahoma has the fourth highest rate of obesity in the nation, at 39.4 percent.3
Many patients experience extreme poverty and live in urban and rural communities where access to healthy and nutritionally dense food is limited. Optimal nutrition is not always seen as accessible in this setting. As healthcare providers, it is our responsibility to dispel this myth and promote healthy nutrition that can be accessible to all patients. That task starts with having direct, informative conversations with patients.
Early in my PA career, my nutrition guidance to patients focused solely on increasing exercise and eating more fruits and vegetables. This advice, though accurate, is inadequate on its own. I now work with patients to create tangible ideas and goals. I recently saw a new patient who had been managing diabetes for a few years and was not well-controlled. With motivational interviewing, I learned that one of his biggest health fears was having to start insulin injections. He and his partner, who had also been diagnosed with diabetes, were shocked to learn that insulin injections were not inevitable. We discussed the importance of nutrition and lifestyle modifications in conjunction with medical management to treat his diabetes.
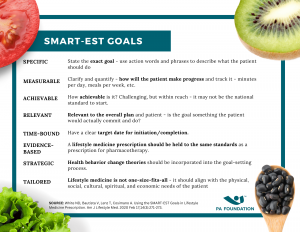
One method I use in my daily practice and teach my students is developing SMART-EST goals. SMART-EST goals are specific, measurable, achievable, relevant, time-bound, evidence-based, strategic, and tailored to a patient.4 For my patient with diabetes, our goals included adding one vegetable to all meals, swapping soda for unsweetened tea, and starting to take 15-minute walks a few times a week. When I saw the patient for a follow-up visit, both he and his partner had implemented these lifestyle changes. They were feeling better, had lost weight, and were motivated to continue to make changes focusing on nutrition and healthy lifestyle choices. This health improvement trend continued throughout our subsequent visits.
As part of this process, it was also exciting to see my student observe the impact of tangible lifestyle changes on the patient’s health. These visits showed the student clinician the importance of assessing nutrition and working with patients to develop attainable goals, which ultimately result in improved health outcomes and well-being. It also highlighted the benefits of continued nutrition education to help with specific diagnoses and treatments, and reinforced that nutrition is a nuanced topic that shouldn’t be simplified to just eating less and exercising more.
We all have stories of patients who have impacted our careers. Though our encounters look different, I imagine connection, education, and nutrition play a role in all of them. As PAs, one of our primary roles is to educate—our students, our patients, and ourselves. With education, let’s empower our patients to make healthy nutrition and lifestyle choices.
Resources
References
- Crowley J, Ball L, Hiddink GJ. Nutrition in Medical Education: A Systematic Review. Lancet Planet Health. 2019; 3: e379-89.
- Nutrition tool kit. American Academy of Physician Associates. Accessed May 5, 2023. https://www.aapa.org/cme-central/national-health-priorities/nutrition-toolkit/
- Adult Obesity Prevalence Maps. Centers for Disease Control and Prevention. Updated September 27, 2022. Accessed May 5, 2023. https://www.cdc.gov/obesity/data/prevalence-maps.html#overall
- White ND, Bautista V, Lenz T, Cosimano A. Using the SMART-EST Goals in Lifestyle Medicine Prescription. Am J Lifestyle Med. 2020 Feb 17;14(3):271-273.

