Using Nutrition as a Surgical Tool
Nicole Fox, MPAS, PA-C
PA Foundation Nutrition Outreach Fellow
November 4, 2021
 For the past year, I have had the pleasure to serve as a Nutrition Outreach Fellow with the PA Foundation. The program offers additional training and resources on nutrition, with the goal of improving individual patient visits as well promoting wellness in our communities. This article reviews a concept called enhanced recovery after surgery, or ERAS, which emphasizes the role of nutrition before and after surgery. Though not a standard part of many pre-operative exams, ERAS is a powerful tool that any provider can use to improve postsurgical outcomes.
For the past year, I have had the pleasure to serve as a Nutrition Outreach Fellow with the PA Foundation. The program offers additional training and resources on nutrition, with the goal of improving individual patient visits as well promoting wellness in our communities. This article reviews a concept called enhanced recovery after surgery, or ERAS, which emphasizes the role of nutrition before and after surgery. Though not a standard part of many pre-operative exams, ERAS is a powerful tool that any provider can use to improve postsurgical outcomes.
Malnutrition, simply defined, refers to any nutritional imbalance. While we often think of frail, thin patients as malnourished, malnutrition can impact any patient of any size (including individuals affected by the chronic disease of obesity). The Academy of Nutrition and Dietetics and the American Society for Parenteral and Enteral Nutrition (ASPEN) consider any individual with two or more of the following factors as malnourished[1]:
- Insufficient energy intake
- Weight loss
- Loss of muscle mass
- Loss of subcutaneous fat
- Localized or generalized edema
- Diminished functional status (e.g. diminished hand grip strength)
Malnutrition is common. Some studies estimate that up to 65% of surgical patients are malnourished[2], with higher prevalence if the patient is undergoing surgery due to cancer or digestive complications (such as malabsorptive conditions). Malnourished patients have a much higher risk of morbidity and mortality associated with their surgery as well. Malnourished individuals are two times more likely to be readmitted within 30 days, three times more likely to have a complication from their surgery, and five times more likely to die after the procedure.[3] This is an issue that can have a significant risk of mortality for our patients!
Malnutrition is reversible, and those of us working in both surgery and primary care have an opportunity to make a difference. There are many preoperative screens that can be used, such as the preoperative nutrition score (PONS)[4] and a 24-hour dietary recall. Many surgical advisory groups, such as the American Society for Enhanced Recovery, also have malnutrition screening tools.
In my practice, we have adapted several of these screening tools to our patient population and use the following screening questions with presurgical patients:
- Have you lost more than 3 kg (6.6 lbs) without trying over the past 3 months?
- Has your ability to eat or tolerate food decreased over the past 3 months for any of the following reasons?
- Loss of appetite
- Digestive problems
- Trouble chewing or swallowing
- Trouble affording food
- (Office staff)
- <65 years and BMI <18.5?
- ≥ 65 years: BMI <20?
Though not an officially validated screening tool, these questions have allowed our office staff to screen patients who may be at risk for malnutrition physiologically or socioeconomically, and refer them to additional nutrition counseling. Other practices may find that additional lab measures, such as low albumin or low vitamin D, may be useful screening tools as well.
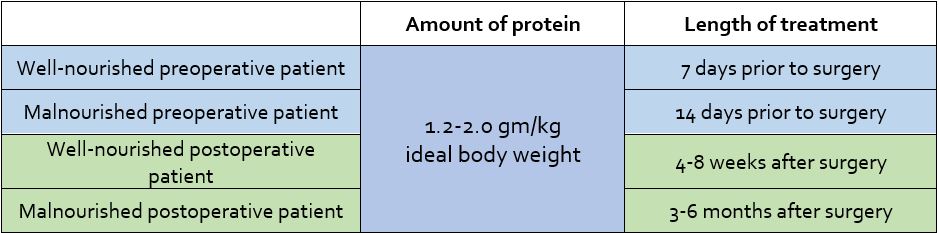
The key to improving presurgical readiness and postsurgical outcomes is increased protein intake. The following general guidelines can be helpful for all patients, regardless of baseline nutritional status[5]:
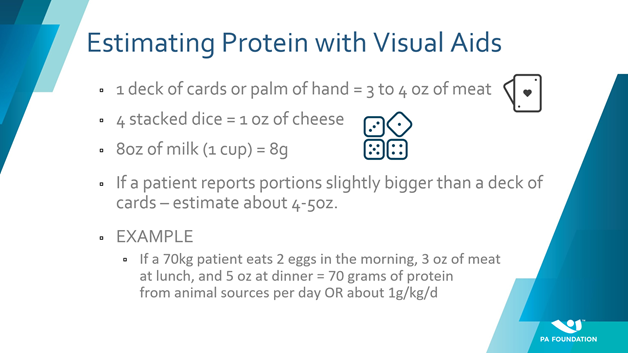
Describing foods with visual aids can be effective in helping patients understand how much protein different foods contain. For example, a 3-4 ounce portion of meat is approximately the size of a deck of cards (see Figure 1). Encouraging high-protein whole foods, such as eggs, and supplements like protein shakes can help patients meet increased nutritional needs surrounding surgery.
Figure 1
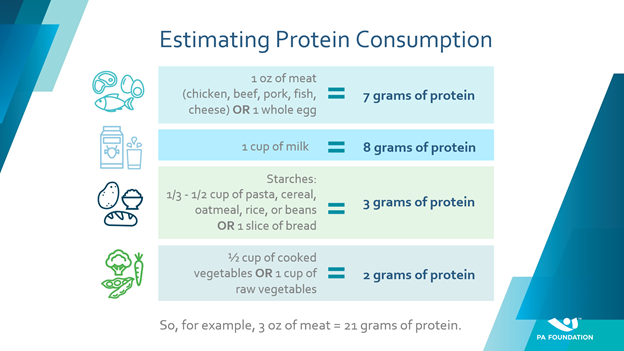
Handouts provided in office can also help patients estimate protein (see Figure 2). For tech-literate patients, apps such as MyFitnessPal or CarbManager provide easy ways to log and track protein intake. Referring to our colleagues in nutrition also helps our patients develop tailored dietary interventions as well as ensure they understand how to make changes at home. For individuals struggling to afford or access high-protein food, incorporating social services or local food relief services can have an enormous impact on their capacity to recover from a procedure.
Figure 2
In summary, nutrition is a powerful predictor of post-surgical outcomes, but is often overlooked. With a few simple questions and tools, we can make a difference in the recovery of every surgical patient we encounter.
Special thanks to Abbott for supporting the Nutrition Outreach Fellowship.
References
[1] Mogensen KM, Malone A, Becker P, et al. Academy of Nutrition and Dietetics/American Society for Parenteral and Enteral Nutrition Consensus Malnutrition Characteristics: Usability and Association With Outcomes. Nutrition in clinical practice: official publication of the American Society for Parenteral and Enteral Nutrition. 2019;34(5):657-665
[2] Wischmeyer PE, Carli F, Evans DC, et al. American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Nutrition Screening and Therapy Within a Surgical Enhanced Recovery Pathway. Anesthesia and analgesia. 2018;126(6):1883-1895.
[3] Awad S, Lobo DN. What’s new in perioperative nutritional support? Curr Opin Anaesthesiol. 2011;24:339–348
Williams JD, Wischmeyer PE. Assessment of perioperative nutrition practices and attitudes—A national survey of colorectal and GI surgical oncology programs. Am J Surg. 2017;213:1010–1018.
Philipson TJ, Snider JT, Lakdawalla DN, Stryckman B, Goldman DP. Impact of oral nutritional supplementation on hospital outcomes. Am J Manag Care. 2013;19:121–128
[4] Gillis C, Wischmeyer PE. Pre-operative nutrition and the elective surgical patient: why, how and what?. Anaesthesia. 2019;74 Suppl 1:27–35. doi:10.1111/anae.14506
[5] Wischmeyer PE, Carli F, Evans DC, et al. American Society for Enhanced Recovery and Perioperative Quality Initiative Joint Consensus Statement on Nutrition Screening and Therapy Within a Surgical Enhanced Recovery Pathway. Anesthesia and analgesia. 2018;126(6):1883-1895.
Weimann A, Braga M, Carli F, et al. ESPEN guideline: Clinical nutrition in surgery. Clin Nutr. 2017;36(3):623–650. doi:10.1016/j.clnu.2017.02.013

